
Kneecap Dislocation
Kneecap (Patella) Dislocation
Kneecap dislocation is a condition affecting adolescents and young people.
It may occur due to a significant force on the knee, such as during a car accident or sporting injury, or it may have occurred simply due to the patient twisting his/her knee or turning his/her body.
Why does Kneecap dislocation happen?
The kneecap is normally held by strong ligaments and muscles around the knee and cannot be pushed out to either side. A kneecap dislocation can happen due to a significant traumatic force, causing tearing of the Medial Patello-Femoral Ligament (MPFL) and causing the kneecap to dislocate to the outer part of the knee.
However, there are several risk factors (also addressed in the page on Patellar Maltracking) that increase the likelihood of this injury happening:
– looseness of knee joint ligaments
– tightness of Ilio-Tibial band
– weak quadriceps muscles
Bony factors may include:
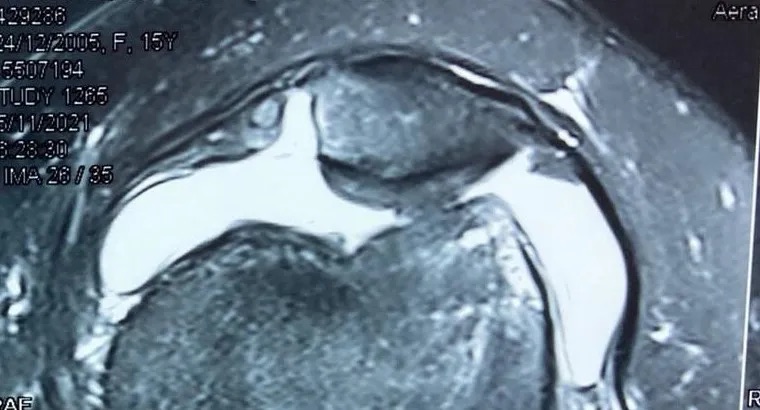
– trochlear dysplasia
– excessive femoral anteversion
– lateralisation of the tibial tubercle
Many of these are complex in-born structural issues of the knee.
Is it going to happen again and again?
Statistically-speaking, about 50% of people who suffer kneecap dislocation only experience it once in their lifetime. The other 50% of people may suffer repeated dislocations.
For people who have recurrent dislocations, they likely have some degree of underlying risk factors, which also pre-disposed to the first episode.
How is kneecap dislocation treated?
The very initial treatment is usually a cast put on the knee to immobilise the knee and the kneecap, allowing swollen soft tissues to settle first. Thereafter, a complete assessment by an Orthopaedic specialist experienced in these issues is important. MRI, Xrays, and CT scan may also be ordered to add to the information about the condition.
If there is no concomitant cartilage injury (called Osteochondral injury), and the knee is assessed to be at low right of subsequent dislocations, then conservative treatment with immobilisation followed by graduated rehab exercises can be undertaken.
If there is an osteochondral injury, a loose body, or the knee is assessed to be at high risk of subsequent dislocations due to the underlying risk factors, then surgical treatment may have to be considered. There is a move towards surgery even for first-time dislocations in cases where there is high risk of subsequent dislocations.
Intermediate cases with MPFL ligament tear and medium risk of subsequent dislocations may be treated with a biological injection to the ligament.

What does surgery for kneecap dislocation involve?
Due to the complexity of this issue, many techniques are available and there is no one surgical technique which has proven to be the best. However, the mainstays of such treatment would likely involve the following:
1) If there is an osteochondral injury, to repair or re-surface the cartilage
2) If there is an osteochondral loose body that cannot be repaired, to remove it
3) Reconstruction of the Medial Patello-Femoral Ligament (MPFL) would likely be the mainstay
4) If there is significant trochlear dysplasia, to re-shape the underlying trochlear bone. This is called a Trochleoplasty (most commonly the Lyon trochleoplasty).
5) If there is significant lateralisation of the tibial tubercle, to shift the tibial tubercle bone, called a Fulkerson osteotomy
What happens if repeated kneecap dislocations is not treated?
Each time the kneecap dislocates, the soft tissues around the kneecap get more damaged and make it even more likely for the next dislocation to happen.
With repeated dislocations, cartilage beneath the kneecap starts to get damaged and there is a significant risk of early-onset arthritis. This causes persisting pain that affects walking and function.
Centurion Orthopaedic Centre
38 Irrawaddy Road
Mt Elizabeth Novena Hospital Specialist Centre #07-40
Singapore 329563









